Data From Phase 3 Pivotal Studies Show Amgen's Novel Investigational Cholesterol-Lowering Medication Evolocumab Significantly Reduced LDL Cholesterol In Statin Intolerant Patients And In Patients On Statins
03.30.2014
|
Evolocumab is an investigational fully human monoclonal antibody that inhibits proprotein convertase subtilisin/kexin type 9 (PCSK9), a protein that reduces the liver's ability to remove LDL-C from the blood.1
In the GAUSS-2 study, the most common adverse events (AEs) (≥5 percent in the combined evolocumab group) were headache, myalgia, pain in extremity and muscle spasms. In the LAPLACE-2 study, no AEs occurred in ≥2 percent of the evolocumab combined group. The most common AEs in the evolocumab combined group (>1.5 percent) were back pain, arthralgia, headache, muscle spasms and pain in extremity.
"As treatment with statins continues to be an important tool in the management of high cholesterol, we are encouraged by the positive data from the Phase 3 studies of evolocumab in patients with statin intolerance and in patients already on statin therapy," said
"Results from the five Phase 3 pivotal studies that we presented at ACC span more than 4,000 patients and provide us with important insights on the potential of evolocumab as a treatment for a range of patients at-risk for cardiovascular disease," Harper added. "We are working closely with regulatory authorities on our global filing plan in hopes of bringing this new treatment option to patients with dyslipidemia."
GAUSS-2 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects-2) Primary Results
- The GAUSS-2 study showed that in 307 patients with high cholesterol who could not tolerate effective doses of at least two different statins due to muscle-related side effects, treatment with subcutaneous evolocumab (140 mg every two weeks or 420 mg monthly), significantly reduced mean LDL-C by 37-39 percent from baseline compared to ezetimibe (p<0.001).
- Results of the study showed the mean percent reduction from baseline in LDL-C at weeks 10 and 12 were 37 percent for evolocumab 140 mg every two weeks and 39 percent for evolocumab 420 mg monthly compared to ezetimibe.
- At week 12, the percent reduction from baseline in LDL-C was 38 percent for evolocumab 140 mg every two weeks and 38 percent for evolocumab 420 mg monthly compared to ezetimibe.
- The most common AEs (>5 percent in evolocumab combined group) were headache (7.8 percent evolocumab; 8.8 percent ezetimibe), myalgia (7.8 percent evolocumab; 17.6 percent ezetimibe), pain in extremity (6.8 percent evolocumab; 1.0 percent ezetimibe) and muscle spasms (6.3 percent evolocumab; 3.9 percent ezetimibe).
"Data from the GAUSS-2 study suggest evolocumab could be a promising lipid-lowering treatment for patients with high cholesterol who cannot tolerate effective doses of statins," said GAUSS-2 lead investigator
LAPLACE-2 (LDL-C Assessment with PCSK9 MonoclonaL Antibody Inhibition Combined with Statin ThErapy-2) Primary Results
- The LAPLACE-2 study showed that in 1,896 patients with high cholesterol (LDL-C >80 mg/dL), treatment with subcutaneous evolocumab (140 mg every two weeks or 420 mg monthly) in combination with different daily doses of statin therapy significantly reduced mean LDL-C by 55-76 percent from baseline compared to placebo and 38-47 percent from baseline compared to ezetimibe (p<0.001).
- Results of the study showed the mean reduction in LDL-C from baseline at weeks 10 and 12 was between 66-75 percent for evolocumab 140 mg every two weeks versus placebo and between 38-45 percent versus ezetimibe, for all statin cohorts.
- Results of the study also showed the mean percent reduction in LDL-C from baseline at weeks 10 and 12 was between 63-75 percent for evolocumab 420 mg monthly versus placebo and 44 percent versus ezetimibe, for all statin cohorts.
- At week 12, the percent reduction from baseline in LDL-C was between 68-76 percent for evolocumab 140 mg every two weeks and between 55-71 percent for evolocumab 420 mg monthly, compared to placebo, for all statin cohorts. Compared with ezetimibe, evolocumab reduced LDL-C from baseline between 40-47 percent when dosed every two weeks and between 39-41 percent when dosed monthly, for all statin cohorts.
- No AEs occurred in ≥2 percent of the evolocumab combined group. The most common AEs in the evolocumab combined group were back pain (1.8 percent evolocumab; 3.2 percent ezetimibe; 2.5 percent placebo), arthralgia (1.7 percent evolocumab; 1.8 percent ezetimibe; 1.6 percent placebo), headache (1.7 percent evolocumab; 2.3 percent ezetimibe; 2.7 percent placebo), muscle spasms (1.5 percent evolocumab; 2.7 percent ezetimibe; 1.1 percent placebo) and pain in extremity (1.5 percent evolocumab; 1.4 percent ezetimibe; 1.3 percent placebo).
"The positive results from the LAPLACE-2 study show that adding evolocumab to statin therapy additionally lowers LDL cholesterol levels when added to moderate or high doses of statins," said LAPLACE-2 lead investigator
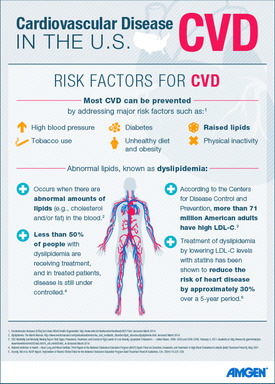
High cholesterol is the most common form of dyslipidemia, which is an abnormality of lipids in the blood.2,3 There are approximately 300 million cases of dyslipidemia in the U.S.,
Live audio of the investor meeting will be simultaneously broadcast over the Internet and will be available to members of the news media, investors and the general public.
The webcast, as with other selected presentations regarding developments in
GAUSS-2 Study Design
GAUSS-2 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects-2) is a Phase 3 randomized, multicenter, double-blind, placebo- and ezetimibe-controlled trial designed to evaluate the safety, tolerability and efficacy of evolocumab in 307 hyperlipidemic patients who could not tolerate effective doses of at least two different statins due to muscle-related side effects. Patients were randomized to one of four treatment groups: subcutaneous evolocumab 140 mg every two weeks and oral placebo daily; subcutaneous evolocumab 420 mg monthly and oral placebo daily; subcutaneous placebo every two weeks and oral ezetimibe 10 mg daily; or subcutaneous placebo monthly and oral ezetimibe 10 mg daily. The co-primary endpoints were the percent reduction from baseline in LDL-C at week 12 and the mean percent reduction from baseline in LDL-C at weeks 10 and 12. Secondary efficacy endpoints included means at weeks 10 and 12 and at week 12 for the following: absolute change from baseline in LDL-C; LDL-C <70 mg/dL; and the percentage change from baseline in non-high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B (ApoB), total cholesterol (TC)/HDL-C ratio, ApoB/apolipoprotein A1 (ApoA1) ratio, lipoprotein(a), triglycerides, HDL-C and very low-density lipoprotein cholesterol (VLDL-C).
LAPLACE-2 Study Design
LAPLACE-2 (LDL-C Assessment with PCSK9 MonoclonaL Antibody Inhibition Combined with Statin ThErapy-2) is a Phase 3 randomized, multicenter, double-blind, placebo- and ezetimibe-controlled study designed to evaluate safety, tolerability and efficacy of evolocumab in 1,896 patients with primary hypercholesterolemia and mixed dyslipidemia (LDL-C ≥80 mg/dL) when added to statin therapy. Patients were randomized to one of 24 treatment groups in a two-step randomization. Eligible patients were initially randomized to one of five open label background statin treatments: atorvastatin 10 mg, atorvastatin 80 mg, rosuvastatin 5 mg, rosuvastatin 40 mg or simvastatin 40 mg daily. Patients randomized to atorvastatin were then randomized to one of six treatment groups: evolocumab every two weeks and oral placebo, evolocumab every month and oral placebo, subcutaneous placebo every two weeks and oral placebo, subcutaneous placebo every month and oral placebo, subcutaneous placebo every two weeks and ezetimibe 10 mg, or subcutaneous placebo every month and ezetimibe 10 mg. Patients randomized to rosuvastatin or simvastatin were then randomized to one of four treatment groups: evolocumab every two weeks, evolocumab every month, subcutaneous placebo every two weeks, or subcutaneous placebo every month.
The co-primary endpoints were the mean percent change from baseline in LDL-C at weeks 10 and 12 and the percent change in LDL-C reduction at week 12. Co-secondary efficacy endpoints included means at weeks 10 and 12 and at week 12 for the following: LDL-C <70 mg/dL; absolute change from baseline in LDL-C; and the percentage change from baseline in non-high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B (ApoB), total cholesterol (TC)/HDL-C ratio, ApoB/apolipoprotein A1 (ApoA1) ratio, lipoprotein(a), triglycerides, HDL-C and very low-density lipoprotein cholesterol (VLDL-C).
About Evolocumab
Evolocumab is a fully human monoclonal antibody that inhibits proprotein convertase subtilisin/kexin type 9 (PCSK9).1 PCSK9 is a protein that targets LDL receptors for degradation and thereby reduces the liver's ability to remove LDL-C, or "bad" cholesterol, from the blood.8 Evolocumab, being developed by
About
The Phase 3 program includes 14 trials to evaluate evolocumab administered every two weeks and monthly in multiple patient populations, including in combination with statins in patients with hyperlipidemia (LAPLACE-2 and YUKAWA-2); in patients with hyperlipidemia who cannot tolerate statins (GAUSS-2 and GAUSS-3); as a stand-alone treatment in patients with hyperlipidemia (MENDEL-2); in patients whose elevated cholesterol is caused by genetic disorders called heterozygous (RUTHERFORD-2 and TAUSSIG) and homozygous (TESLA and TAUSSIG) familial hypercholesterolemia; as well as the administration of evolocumab (THOMAS-1 and THOMAS-2).
Five studies in the evolocumab Phase 3 program will provide long-term safety and efficacy data. These include FOURIER (Further Cardiovascular OUtcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk), which will assess whether treatment with evolocumab in combination with statin therapy compared to placebo and statin therapy reduces recurrent cardiovascular events in approximately 22,500 patients with cardiovascular disease; DESCARTES (Durable Effect of PCSK9 Antibody CompARed wiTh PlacEbo Study) in patients with hyperlipidemia at risk for cardiovascular disease; OSLER-2 (Open Label Study of Long TERm Evaluation Against LDL-C Trial-2) in patients with high cholesterol who completed any of the Phase 3 studies; GLAGOV (GLobal Assessment of Plaque ReGression with a PCSK9 AntibOdy as Measured by IntraVascular Ultrasound), which will determine the effect of evolocumab on coronary atherosclerosis in approximately 950 patients undergoing cardiac catheterization; and TAUSSIG (Trial Assessing Long Term USe of PCSK9 Inhibition in Subjects with Genetic LDL Disorders), which will assess the long-term safety and efficacy of evolocumab on LDL-C in patients with severe familial hypercholesterolemia.
About
About
For more information, visit www.amgen.com and follow us on www.twitter.com/amgen.
Forward-Looking Statements
This news release contains forward-looking statements that are based on management's current expectations and beliefs and are subject to a number of risks, uncertainties and assumptions that could cause actual results to differ materially from those described. All statements, other than statements of historical fact, are statements that could be deemed forward-looking statements, including estimates of revenues, operating margins, capital expenditures, cash, other financial metrics, expected legal, arbitration, political, regulatory or clinical results or practices, customer and prescriber patterns or practices, reimbursement activities and outcomes and other such estimates and results. Forward-looking statements involve significant risks and uncertainties, including those discussed below and more fully described in the Securities and Exchange Commission (
No forward-looking statement can be guaranteed and actual results may differ materially from those
In addition, sales of our products (including products of our wholly-owned subsidiaries) are affected by the reimbursement policies imposed by third-party payers, including governments, private insurance plans and managed care providers and may be affected by regulatory, clinical and guideline developments and domestic and international trends toward managed care and healthcare cost containment as well as U.S. legislation affecting pharmaceutical pricing and reimbursement. Government and others' regulations and reimbursement policies may affect the development, usage and pricing of our products. In addition, we compete with other companies with respect to some of our marketed products as well as for the discovery and development of new products. We believe that some of our newer products, product candidates or new indications for existing products, may face competition when and as they are approved and marketed. Our products may compete against products that have lower prices, established reimbursement, superior performance, are easier to administer, or that are otherwise competitive with our products. In addition, while we and our partners routinely obtain patents for products and technology, the protection of our products offered by patents and patent applications may be challenged, invalidated or circumvented by our competitors and there can be no guarantee of our or our partners' ability to obtain or maintain patent protection for our products or product candidates. We cannot guarantee that we will be able to produce commercially successful products or maintain the commercial success of our existing products. Our stock price may be affected by actual or perceived market opportunity, competitive position, and success or failure of our products or product candidates. Further, the discovery of significant problems with a product similar to one of our products that implicate an entire class of products could have a material adverse effect on sales of the affected products and on our business and results of operations. Our efforts to integrate the operations of companies we have acquired may not be successful.
The scientific information discussed in this news release related to our product candidates is preliminary and investigative. Such product candidates are not approved by the U.S. Food and Drug Administration (
CONTACT:
References
- Amgen Data on File, Investigator Brochure.
World Health Organization . Quantifying Selected Major Risks to Health. In: The World Health Report 2002 - Reducing Risks, Promoting Healthy Life. Chapter 4:Geneva :World Health Organization ;202:47-97.- Merck Manuals website. http://www.merckmanuals.com/professional/endocrine_and_metabolic_disorders/lipid_disorders/dyslipidemia.html. Accessed
March 2014 . National Institute of Health (2006). Federal Register Volume 74 (250).Washington, DC : U.S. Government Printing Office. http://www.gpo.gov/fdsys/pkg/FR-2009-12-31/html/E9-31072.htm. AccessedMarch 2014 .- CDC Morbidity and Mortality Weekly Report.
Vital Signs : Prevalence, Treatment, and Control of High Levels of Low-Density Lipoprotein Cholesterol ---United States , 1999--2002 and 2005-2008.February 4, 2011 . Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6004a5.htm?s_cid=mm6004a5_w. AccessedMarch 2014 . American Heart Association (2012). Why cholesterol matters. http://www.heart.org/HEARTORG/Conditions/Cholesterol/WhyCholesterolMatters/Why-Cholesterol-Matters_UCM_001212_Article.jsp. AccessedMarch 2014 .World Health Organization . Global status report on noncommunicable diseases 2010.Geneva , 2011.- Abifadel M et al.
Nat Genet . 2003;34:154-156.

To view the multimedia assets associated with this release, please click: http://www.multivu.com/mnr/7061855-amgen-at-american-college-of-cardiology-acc-14-march-30
SOURCE
